|
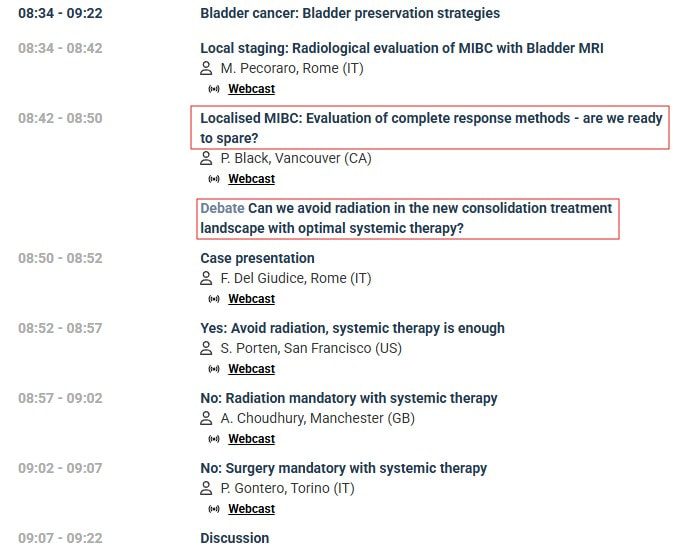
I listened recently to a plenary session of great interest to me at the 40th annual European Association of Urology congress. [I appreciate the work of the EAU and joined as a patient advocate member, in part to access such content.] The topic was bladder sparing strategies - in particular, in cases where a complete response is observed after transurethral resection of the bladder tumor (TURBT) and neoadjuvant systemic therapy- Is active surveillance a safe option? As this is my strategy - my interest was piqued. The discussion was framed around a case study with localized muscular invasive bladder cancer (MIBC). Unlike my case - in this case PET/CT found no spread of disease into local lymph nodes - so the context of the discussion was localised MIBC. However with current treatments and diagnostics, I believe the discussion is applicable to my case of locally advanced MIBC. Dr. Black posed the question: Do we have tools to determine a complete response? One of the studies cited (RETAIN 1) I had mentioned an earlier post. Patients selected for this trial presented with at least one of a set of genetic mutations - including ERCC2. The neoadjuvant chemotherapy was AMVAC . [This study was initiated before the approval of my treatment - enfortumab vedotin and pembrolizumab (EV+pembro).] Active surveillance included imaging but the study was done prior to the emergence of circulating tumor DNA (ctDNA) which I rely on. I had a low mutation burden based on genetic analysis of my tumor, but ERRC2 was found as a likely pathogenic variant. ERCC2 is associated with sensitivity to treatment with cisplatin-based chemotherapy but recently has also been shown to be an independent predictor of favorable progonosis for bladder cancer. I also had a CPS score of 10 for PD-L1. A score of 10 or greater suggest a higher likelihod of benefit from pembrolizumab. However, there is currently no patient selection for EV+pembro by biomarker as none have been shown to be sufficiently predictive of positive response - EV+pembro is approved as an "all comers" first line option for patients with locally advanced or metastatic muscle invasive bladder cancer. In the RETAIN 1 trial, all patients chose to try and preserve their bladder - 48% of the patients who had a complete response remained metatasis-free with intact bladder. In the EV 302 trial which led to approval of my treatment - 38% of the participants had a complete pathological response. The literature does not cite how many (if any) of those patients retained their bladder - but Dr. Black expected that with the advent of new systemic treatments like EV+pembro, more patients (like me) with a complete pathological response, may choose to maintain their bladder and begin active surveillance after systemic treatment. Dr. Black listed a number of tools for determining complete response (see Figure 2). In addition to my toolset, MRI was mentioned - multiparmetric MRI (mpMRI) and new VI-RAD protocools in particular. The first talk in the session presented recent evidence of accuracy of MR for local staging and detecting local recurrence. I lead software development for the first generations of PET/CT and I have confidence PET/CT to detect metastatic disease (it found spread to my pelvic lymph nodes), but I believe my first indication of recurrence will be from ctDNA. Urine circulating tumor DNA was also mentioned but its effectiveness is still being assessed. It was noted that patients (as in the RETAIN 1 trial) who experience recurrence can still undergo radical cystectomy or radiation or potentially second line systemic treatments (see Figure 1). The survival with recurrence in the RETAIN 1 trial was similar to other trials where patients underwent radical cystectomy or trimodality therapy immediately after neoadjuvant systemic therapy. Of course, my hope is that, with EV+pembro, complete pathological response proves to be durable and more patients will elect experiencing it will choose to retain their bladder. The next presentation argued for this strategy- first presenting motivation based on an analysis patient concerns {see Figure 3) compilied in a study from the Bladder Cancer Advocacy Network (BCAN). Dr. Porten based her recommendations (see Figure 4) based on recent trials and indicated possibilities of pursuing them in the follow up to the EV302 trial currently in progress. The next two speakers presented the more common choices (and standard of care if disease has not spread outside the bladder) of radical cystectomy or trimodality therapy (TMT) - radiation and chemotherapy. I also lead software development for a proton therapy system and believe, as was presented by Dr. Choudhury (see Figure 5), that evidence is showing that survival with trimodality therapy is not inferior and may actually be slight better than cystectomy. [I was originally planning on trimodality therapy with proton therapy before learning of the results and approval of EV+pembro.] Dr. Gontero presented arguments for the most common choice with MIBC of radical cystectomy. He identified indications which he saw as contraindications to TMT (see Figure 6). He also argued that RC (with adjuvant systemic therapy) was the best option for long term recurrence free survival for localised disease. Certainly there is a larger body of longer term follow up data as this has been the dominant strategy. I am encouraged to see more presentations like these. The trend in the community, with continuing improvements in treatments and surveillance diagnostics, is pointing to more bladder sparing.
In support of building evidence to include bladder sparing following TURBT and complete pathological response to neoadjuvant treatment, I would like to see the creation of a registry of data of patients who have followed this strategy - more details in my next post...
4 Comments
With my most recent CT scan continuing to show no sign of progression and my circulating tumor DNA tests showing no evidence of disease, my oncologist informed me that my Keytruda (pembrolizumab) infusions can stop at 36 (2 years). This first 7 infusions were part of 7 cycles of Padcev (enfortumab vedotin - 14 infusions) and Keytruda. This duration was determined in the KEYNOTE trials of Keytruda with various cancers including advanced urothelial cell carcinoma.
I began treatment on Dec 11, 2023 - 36 Keytruda infusions brings me to Dec 19, 2025. A nurse in the infusion suite said that they will miss me but will celebrate that day with me. Here's to a Merry Christmas after 14 more sessions in the chair. |
AuthorI began a health journey in the fall of 2017 - losing 100 lbs and reversing type II diabetes. Archives
March 2025
Categories |






 RSS Feed
RSS Feed